The Shifting Landscape of Obesity Treatment: Navigating the Price and Access Challenges of Wegovy and Zepbound
The emergence of GLP-1 receptor agonists like Wegovy and Zepbound has revolutionized obesity treatment, offering a new avenue for individuals struggling with weight management. These medications have witnessed a surge in popularity, demonstrating promising results in clinical trials and real-world applications. However, despite their efficacy, access to these groundbreaking drugs remains a complex issue, fraught with financial hurdles and inconsistent insurance coverage.
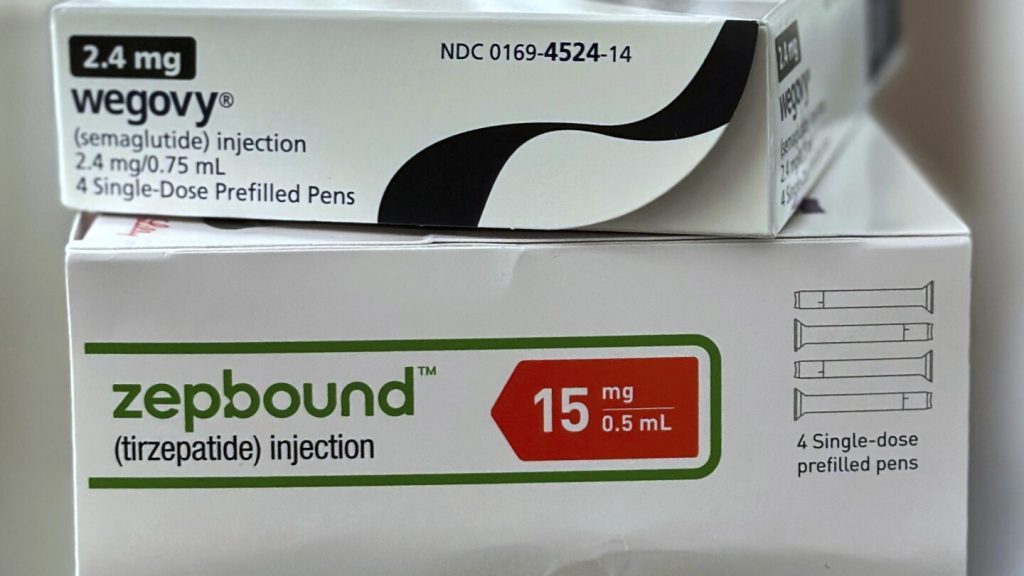
The Obesity Treatment Revolution: A Glimpse into Wegovy and Zepbound
Wegovy, manufactured by Novo Nordisk, and Zepbound, produced by Eli Lilly, belong to a class of medications known as GLP-1 receptor agonists. These drugs mimic the effects of a natural hormone called glucagon-like peptide-1 (GLP-1), which plays a crucial role in regulating appetite and blood sugar levels. By activating GLP-1 receptors in the brain, these medications can effectively reduce hunger, increase feelings of fullness, and ultimately lead to weight loss.
The success of Wegovy and Zepbound is evident in their impressive sales figures. Zepbound generated a staggering $2.3 billion in U.S. sales during the first quarter of this year, solidifying its position as one of Eli Lilly’s top-performing drugs. Similarly, Novo Nordisk reports approximately 200,000 weekly prescriptions for Wegovy in the U.S., contributing to nearly $1.9 billion in first-quarter sales. These numbers underscore the high demand for these medications and their potential to transform the landscape of obesity treatment.
The Price Barrier: A Significant Obstacle to Access
Despite their effectiveness, the high cost of Wegovy and Zepbound remains a significant barrier for many individuals seeking obesity treatment. Even with recent price reductions, these medications still cost around $500 per month for those without insurance, rendering them unaffordable for a large segment of the population. This financial burden disproportionately affects individuals from lower socioeconomic backgrounds, who often face the greatest challenges in accessing healthcare services.
The cost issue extends beyond those without insurance. Even individuals with insurance coverage may face substantial out-of-pocket expenses, as many plans only cover a portion of the medication’s cost. This can leave patients with hundreds of dollars in monthly costs, making it difficult to sustain long-term treatment. While drug manufacturers offer assistance programs to help offset these costs, the eligibility criteria and coverage limits can be restrictive, leaving many patients struggling to afford the medications they need.
The Uneven Terrain of Insurance Coverage: A Patchwork of Policies
Insurance coverage for Wegovy and Zepbound remains inconsistent, creating further obstacles to access. While some employers and insurance companies are expanding their coverage of these medications, many others still exclude them from their formularies. This inconsistency stems from concerns about the long-term costs of these medications and the potential for widespread use.
Mercer, a benefits consulting firm, reports that more businesses with 500 or more employees are adding coverage for the injected drugs for their workers and family members. Novo Nordisk also claims that 85% of its patients with coverage in the U.S. pay $25 or less per month. However, these figures do not represent the entire picture.
Most state and federally funded Medicaid programs do not cover Wegovy and Zepbound for obesity, and neither does Medicare, the federal program primarily for individuals aged 65 and older. This lack of coverage disproportionately affects vulnerable populations who rely on these programs for their healthcare needs.
Even when insurance plans cover Wegovy and Zepbound, the coverage may be limited or require prior authorization. This can involve a lengthy and complex process, requiring patients to provide extensive documentation to justify their need for the medication. These hurdles can discourage patients from pursuing treatment or delay their access to these potentially life-changing drugs.
The PBM Factor: Influencing Access Through Formulary Decisions
Pharmacy benefit managers (PBMs) play a significant role in determining which medications are covered by insurance plans. PBMs negotiate drug prices with manufacturers and create formularies, which are lists of covered drugs. These formulary decisions can have a profound impact on patient access to medications like Wegovy and Zepbound.
Recently, CVS Health, one of the nation’s largest PBMs, dropped Zepbound from its national formulary in favor of Wegovy. This decision means that millions of individuals covered by CVS Health plans will no longer have access to Zepbound, potentially forcing them to switch to Wegovy or explore alternative treatment options.
Such decisions highlight the complex dynamics between drug manufacturers, PBMs, and insurance companies, and how these dynamics can impact patient access to essential medications. While PBMs argue that formulary decisions are based on cost-effectiveness and clinical efficacy, critics contend that they prioritize profits over patient needs.
The Compounding Conundrum: A Cheaper Alternative with Safety Concerns
Compounding pharmacies offer a potential alternative to brand-name medications like Wegovy and Zepbound. Compounding involves creating customized medications by combining, mixing, or altering ingredients. During periods of drug shortages, compounding pharmacies were allowed to make off-brand, cheaper copies of Wegovy and Zepbound.
However, the FDA has determined that the shortage of these drugs has ended, which should have curtailed the practice of compounding. Despite this, some compounding is still permitted when a drug is personalized for the patient. This exception has led to the emergence of companies like Hims & Hers Health, which offer compounded doses of semaglutide, the active ingredient in Wegovy.
These compounded versions are often significantly cheaper than the brand-name drugs, making them an attractive option for individuals who cannot afford Wegovy or Zepbound. However, the safety and efficacy of compounded drugs are not always guaranteed.
Novo Nordisk has raised concerns about the quality and safety of compounded versions of its drug, citing the use of ingredients from foreign suppliers not monitored by U.S. regulators. The company ended a partnership with Hims due to concerns about the company’s continued compounding practices.
While companies like Hims assert that they adhere to stringent quality control measures and verify the strength of their compounded drugs through third-party testing, the lack of FDA oversight raises concerns about the consistency and reliability of these products. Patients considering compounded versions of Wegovy or Zepbound should carefully weigh the potential risks and benefits and consult with their healthcare providers.
The Path Forward: Towards Affordable and Accessible Obesity Treatment
Addressing the challenges surrounding access to Wegovy and Zepbound requires a multi-faceted approach involving drug manufacturers, insurance companies, PBMs, and government agencies.
Drug manufacturers can play a role by lowering the prices of their medications and expanding patient assistance programs. Insurance companies can broaden their coverage of Wegovy and Zepbound and streamline the prior authorization process. PBMs can prioritize patient needs over profits when making formulary decisions. Government agencies can explore policy options to increase access to obesity treatment, such as expanding Medicaid and Medicare coverage.
The development of oral versions of GLP-1 receptor agonists could also help drive down prices and improve access. These oral medications are likely to be more convenient and less expensive than the injectable versions, potentially making them more accessible to a wider range of patients.
Furthermore, increased competition among drug manufacturers could help lower prices. As more companies enter the market with similar medications, price wars may ensue, benefiting consumers.
A Note of Optimism: Hope for the Future
Despite the current challenges, there is reason for optimism regarding the future of obesity treatment. The development of new medications, the expansion of insurance coverage, and the potential for increased competition all point towards a future where effective obesity treatment is more affordable and accessible.
As Dr. Courtney Younglove aptly puts it, “I think price wars are going to drive it down. I think we are in the early stages. I have hope.”
The journey towards affordable and accessible obesity treatment is ongoing, but with continued innovation, collaboration, and a commitment to patient well-being, we can create a future where everyone has the opportunity to achieve a healthy weight and improve their overall quality of life.
Objective Analysis: The high cost of these medications raises questions about healthcare equity. While these drugs offer a significant benefit, their high price point could exacerbate health disparities, limiting access to those who need them most. It’s crucial for stakeholders to consider the ethical implications of pricing strategies and ensure that effective treatments are accessible to all, regardless of socioeconomic status.